What’s the point of asking patients or the public about their thoughts on AI being used in healthcare?
Dr Lauren Gatting (Queen Mary, University of London) and Dr Charlotte Wahlich (City St George’s, University of London)
July 29, 2024
As researchers, we both conduct work looking at patient and public perceptions of Artificial Intelligence (AI) being used in healthcare.
For Charlotte, this has included exploring patients’ and healthcare professionals’ thoughts and perceptions around the potential use of AI to detect diabetic eye disease in the Diabetic Eye Screening Programme 1. For Lauren, the focus has been on AI being used to inform when to invite people for breast cancer screening [2]. Use of AI in healthcare is currently in the development and implementation stages, with rapid advancements in these technologies expected to continue. This will have a significant impact on healthcare systems and patients’ healthcare pathways. The earlier patients and public voices can be heard and incorporated into the development and implementation of, and communication strategies surrounding, AI in healthcare, the better.
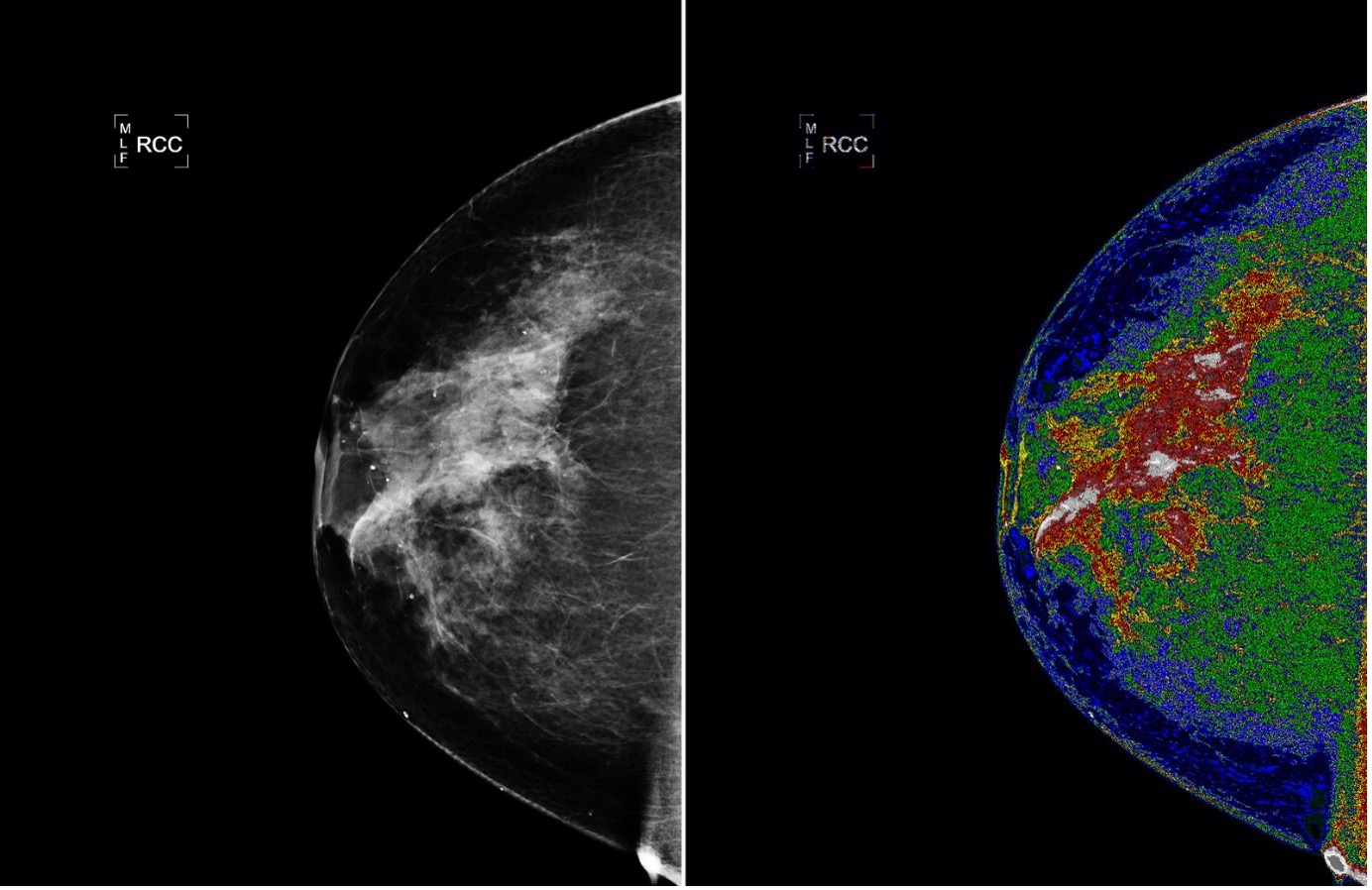 Photo from NASA Goddard Space Flight Center
Photo from NASA Goddard Space Flight Center
When reporting our work to both academic and public audiences, we often get asked the question ‘but why bother asking patients about the use of AI in healthcare?’
This perspective often stems from the following beliefs: 1) AI will and should be implemented into healthcare if it proves to be clinically effective (i.e. improves the care and health outcomes of patients and service users), irrespective of patient and public opinion, and 2) patients do not need to be informed about AI use in healthcare systems if they are not directly interacting with it, like their lack of knowledge about specific blood testing machines or administrative software. In this blog post, we aim to persuade you of the importance of understanding patient and public perceptions of AI healthcare technologies by outlining our key reasons for doing so.
Our first set of reasons are value-based, with ethical underpinnings. We hold the stance that moral and ethical reasons are enough of a justification to carry out research into patient and public perceptions of AI use in healthcare.
- Involvement
Patients have the right to know about the AI applications being used in their healthcare 3 – with the ‘involvement of all stakeholders in the development of AI systems’ being an important consideration in AI research 4. Our current work aims to engage the population in decision-making and to improve understanding about the upcoming changes. This approach fosters trust and ethical practices, ultimately leading to greater equality in healthcare, with all taking part and benefiting from the use of AI in their care. It is our obligation as researchers, alongside healthcare professionals and decision makers, to provide patients with the opportunity to share their perspectives on decisions that are going to impact them. - Transparency
Transparency is key to building trust among patients, healthcare providers and other stakeholders 5. If we can foster trust, accountability and continuous improvement, this will ultimately lead to better health outcomes which will support public confidence in these advanced technologies. Hence, open communication about how and why AI tools are being used is vital to prevent any breakdown of trust in healthcare. - Data ownership
Patients have the right to know, and consent to, how their data are being used or shared. As the development, testing and running of AI all rely on the processing of patient data, it is important that we understand whether patients consider this use of their data acceptable. Presently, laws do not fully protect health data, and data systems are vulnerable to cyber-attacks 6. Therefore, it is important that patients know what they are consenting to in terms of what data are being collected and how it is going to be used. Additionally, it’s important that we identify and understand patients’ anxieties around serious, but largely preventable, events such as data leaks, so that communications can address these concerns. - Informed decisions and choice
Refinement of patient consent processes to align with AI use will be essential. Ensuring that patients can make informed decisions about their care is a fundamental aspect of medical ethics and patient autonomy - a key component of effective consent being patient education. Patients, therefore should be provided with transparent and accessible information about how AI technologies are being used in their care, including the benefits, risks, and limitations of AI technologies 7. - Patient empowerment
Patient empowerment is a concept founded on the belief that individuals have the right to be personally involved in their healthcare journey 8. When patients are actively involved in their care, they are better equipped to make informed decisions, leading to improved health outcomes and greater satisfaction 9. Empowerment means providing patients with access to their health data, facilitating meaningful conversation about their health, and providing them with proactive health management tools. It also involves encouraging open communication and shared decision-making, ensuring that patients’ values and preferences are respected.
Our second set of reasons for researching perceptions of AI healthcare technologies are outcome-based, focusing on improvements that can be achieved through conducting this research and analysing the findings.
- Better communication leading to better care
By carrying out research into patient and public awareness, understanding, and attitudes towards the use of AI in healthcare, we can inform better communication strategies and tailor educational needs. Given the capabilities and reliability of AI technologies are difficult to judge for nonexperts, time and effort should be given to determining suitable ways of communicating these to patients. It will be similarly challenging to communicate the potential cost-saving of using AI systems. Being able to deliver better communication around use of AI in healthcare will lead to several improved outcomes for the health and care of patients:
- Increased engagement with information and improved understanding will support informed choice;
- Reducing patient fears and concerns will decrease the likelihood of patients avoiding healthcare settings where AI technologies and systems are being used;
- More supportive communication around data processing and protection will help patients understand their rights, including their right to withdraw consent;
- If patients understand how AI is being used in their treatment, they may feel more comfortable and empowered in their healthcare journey.
- Creating fairer systems
Fairness is a critical concept gaining considerable traction in AI applications in healthcare 10, and collects the principles of equity, justice and an absence of bias. Ensuring that AI systems operate fairly is essential to avoid existing biases and inequalities in healthcare 11. Fairness concerns arise if AI does not perform adequately for specific patients 10. Patients are often uniquely positioned to identify situations of bias, both before and during the implementation of AI technologies. Their first-hand experiences and perspectives can identify differences that might not be apparent through data analysis alone. By actively involving patients in the development and monitoring of AI systems, healthcare providers can better detect and address potential biases, ensuring that these advanced tools serve all patients fairly. By openly sharing how these systems operate with patients, they can help identify and tackle biases within the AI algorithms that clinicians and developer may otherwise not see. Additionally, involving patients and hearing their perspective on their healthcare journey can highlight gaps in knowledge and trust brought about by historic and discriminatory practices which would help reduce these gaps and avoid propagating or generating new biases. - Influence implementation decision and policy
The public and patients are key stakeholders, and their perspectives are crucial for improving quality, in healthcare policy and decision making. Incorporating their views can help develop best clinical practices and ensure a smooth implementation process 12. In the context of AI in healthcare, it is important for healthcare professionals to evaluate whether the use of AI will undermine trust in their competence and find ways to avoid this. Empowering the public by researching their perspectives enables data-driven decisions through the swift and accurate analysis of large healthcare data sets. This leads to more precise diagnostics, personalised treatment plans, and improved patient outcomes.
 Photo by Accuray on Unsplash
Photo by Accuray on Unsplash
If you were previously uncertain about the necessity of researching patient and public perceptions of AI in healthcare, we hope to have convinced you that such research is vital for maintaining ethical and moral standards, as well as ensuring high-quality healthcare. Through this research, we can:
- make patient/public voices heard
- cultivate systems that are ethical and promote trust
- inform more acceptable and successful implementation, and
- improve our communications surrounding the use of AI in healthcare.
To continue this discussion or for any comments please contact Charlotte (cwahlich@sgul.ac.uk) or Lauren (l.gatting@qmul.ac.uk).
References
- Willis, K., et al., What are the perceptions and concerns of people living with diabetes and National Health Service staff around the potential implementation of AI-assisted screening for diabetic eye disease? Development and validation of a survey for use in a secondary care screening setting. BMJ Open, 2023. 13(11): p. e075558.
- Gatting, L.S., A; Meccheri, P; Newlands, R; Kehagia, AA; Waller, J Acceptability of artificial intelligence in breast screening: Focus groups with the screening-eligible population in England. BMJ Public Health, Under rewiew.
- Kovarik, C.L., Patient Perspectives on the Use of Artificial Intelligence. JAMA Dermatol, 2020. 156(5): p. 493-494.
- Bernal, J. and C. Mazo, Transparency of Artificial Intelligence in Healthcare: Insights from Professionals in Computing and Healthcare Worldwide. Applied Sciences, 2022. 12(20): p. 10228.
- Cutillo, C.M., et al., Machine intelligence in healthcare—perspectives on trustworthiness, explainability, usability, and transparency. npj Digital Medicine, 2020. 3(1): p. 47.
- Farhud, D.D. and S. Zokaei, Ethical Issues of Artificial Intelligence in Medicine and Healthcare. Iran J Public Health, 2021. 50(11): p. i-v.
- Sharma, M., et al., Artificial Intelligence Applications in Health Care Practice: Scoping Review. J Med Internet Res, 2022. 24(10): p. e40238.
- Agner, J. and K.L. Braun, Patient empowerment: A critique of individualism and systematic review of patient perspectives. Patient Education and Counseling, 2018. 101(12): p. 2054-2064.
- Krist, A.H., et al., Engaging Patients in Decision-Making and Behavior Change to Promote Prevention. Stud Health Technol Inform, 2017. 240: p. 284-302.
- Ueda, D., et al., Fairness of artificial intelligence in healthcare: review and recommendations. Japanese Journal of Radiology, 2024. 42(1): p. 3-15.
- Moore, C.M., The challenges of health inequities and AI. Intelligence-Based Medicine, 2022. 6: p. 100067.
- Pizzo, E., et al., Patient and public involvement: how much do we spend and what are the benefits? Health Expectations, 2015. 18(6): p. 1918-1926.



